We're growing! Find your way while visiting the ACH campus. Learn more >
We're growing! Find your way while visiting the ACH campus. Learn more >

Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2023-2024.

Sign up online to quickly and easily manage your child's medical information and connect with us whenever you need.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

Our ERs are staffed 24/7 with doctors, nurses and staff who know kids best – all trained to deliver right-sized care for your child in a safe environment.

Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2023-2024.

Find health tips, patient stories, and news you can use to champion children.

Our flu resources and education information help parents and families provide effective care at home.

We are dedicated to caring for children, allowing us to uniquely shape the landscape of pediatric care in Arkansas.
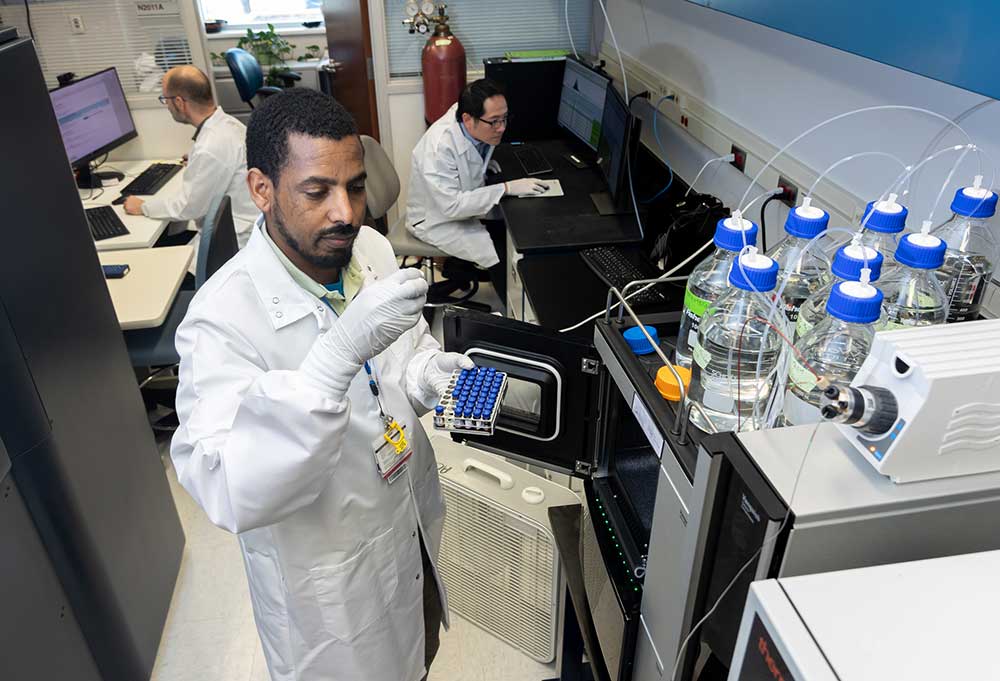
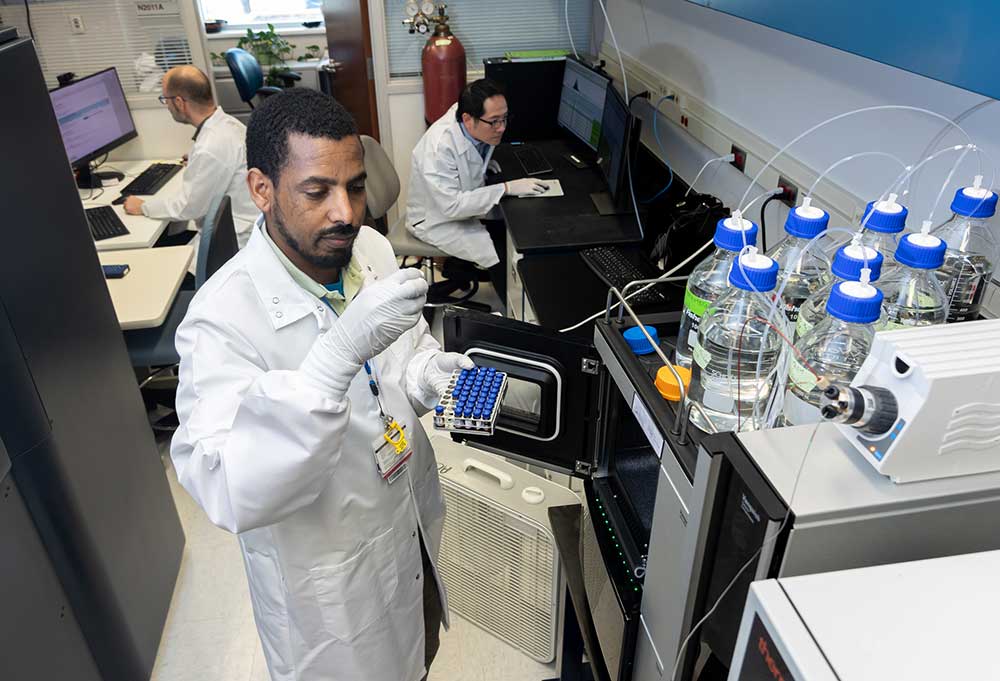
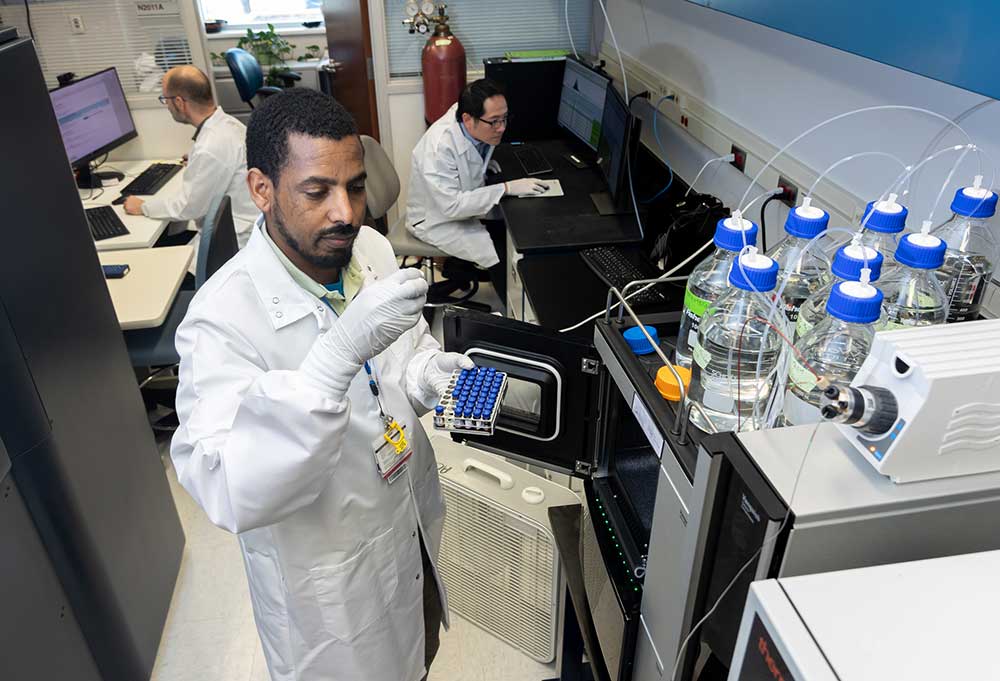
Our researchers are driven by their limitless curiosity to discover new and better ways to make these children better today and healthier tomorrow.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

Then we're looking for you! Work at a place where you can change lives...including your own.

When you give to Arkansas Children's, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond

The gift of time is one of the most precious gifts you can give. You can make a difference in the life of a sick child.

Support and participate in this advocacy effort on behalf of Arkansas’ youth and our organization.
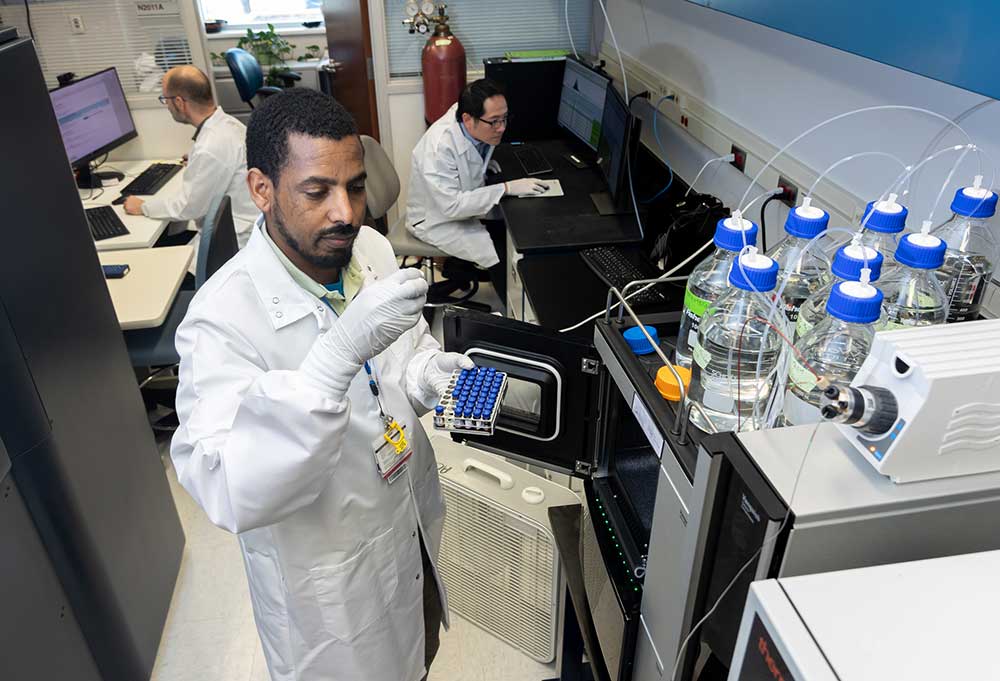
Scientific discoveries lead us to new and better ways to care for childlren.
Scientific discoveries lead us to new and better ways to care for childlren.
Scientific discoveries lead us to new and better ways to care for childlren.
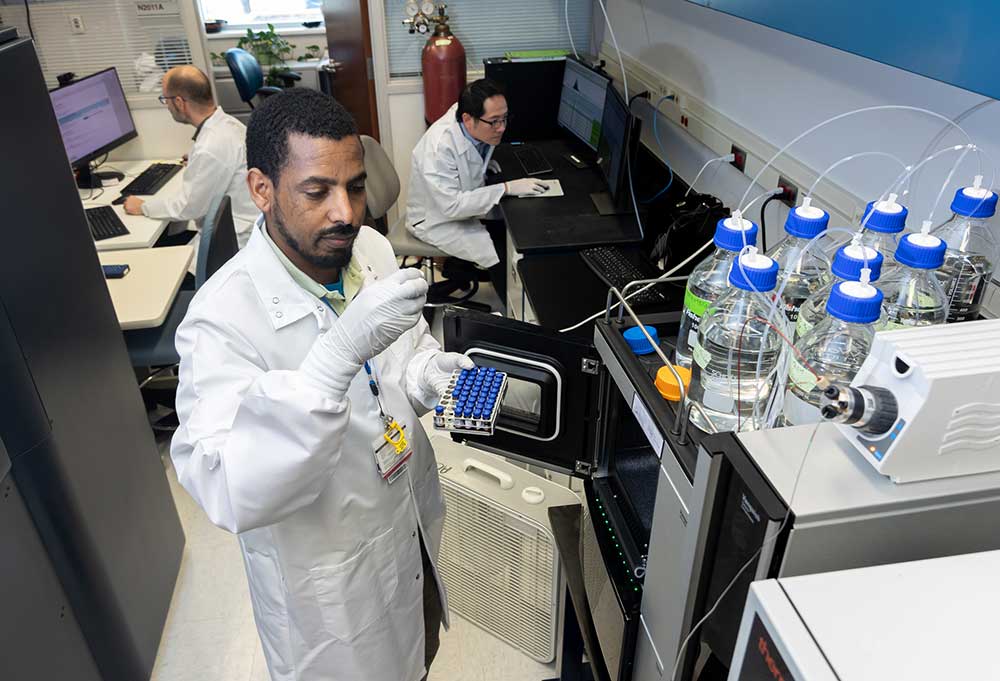
Scientific discoveries lead us to new and better ways to care for childlren.
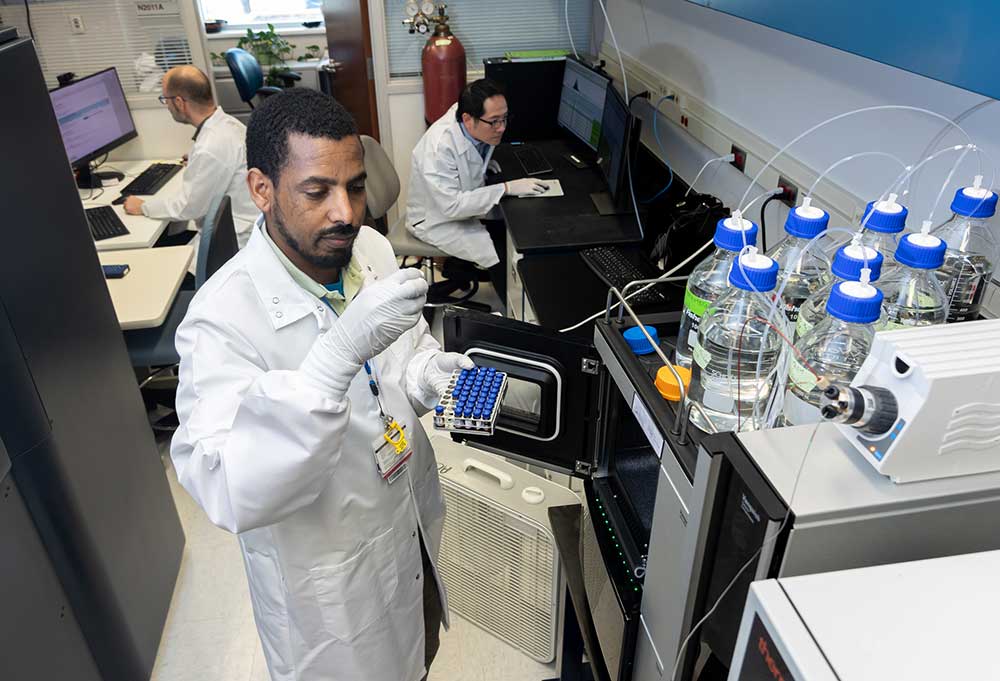
Scientific discoveries lead us to new and better ways to care for childlren.
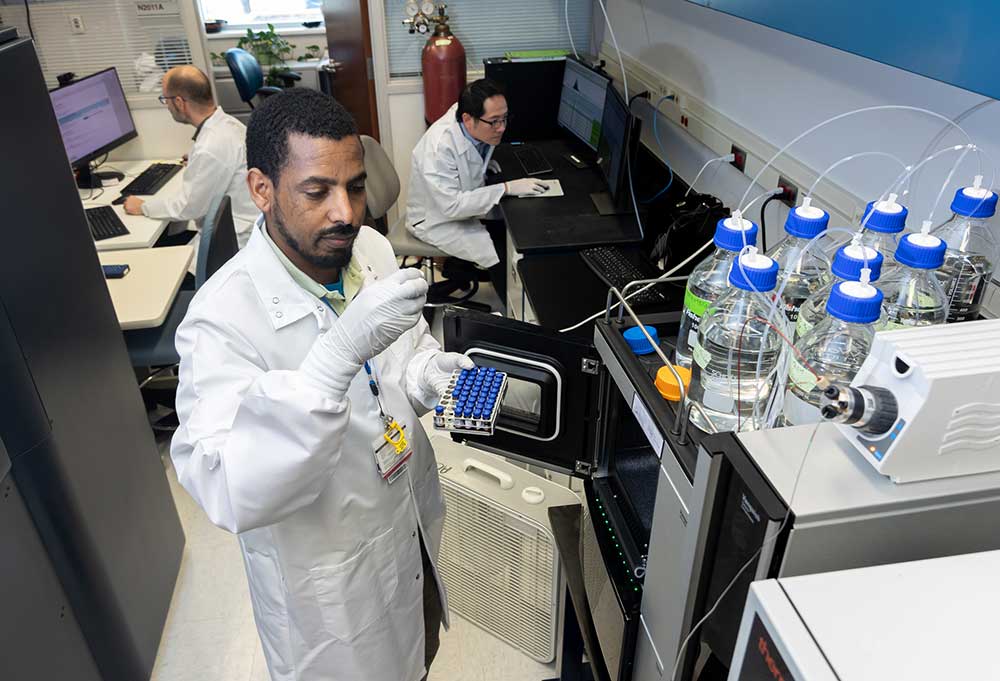
Scientific discoveries lead us to new and better ways to care for childlren.

When you give to Arkansas Children’s, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond.

Your volunteer efforts are very important to Arkansas Children's. Consider additional ways to help our patients and families.

There are many ways to get involved to champion children statewide.

The generosity of our supporters allows Arkansas Children's to deliver on our promise of making children better today and a healthier tomorrow.

Read and watch heart-warming, inspirational stories from the patients of Arkansas Children’s.
Manage your child's medical information and connect with your Arkansas Children's medical team online.
Login Sign upArkansas Children's Hospital
General Information 501-364-1100
Arkansas Children's Northwest
General Information 479-725-6800
Rheumatology refers to inflammatory diseases that affect muscles, joints and connective tissues. These conditions often start with bone and joint pain. Often, a problem with the body’s immune system causes it to attack its own cells. That is why many rheumatic conditions are called autoimmune. The pediatric rheumatology specialists at Arkansas Children’s are specially trained to care for children with conditions more often associated with adults.
If your child has pediatric arthritis or another connective tissue disease, you may be worried about how to ease your child’s pain.
We treat many children with pediatric arthritis as well as children with a wide range of common and rare rheumatic conditions. At Arkansas Children’s, our pediatric rheumatology doctors are experts in diagnosing and treating these conditions.
Our pediatric specialists at Arkansas Children’s provide advanced care for many conditions affecting children of all ages, including:
Chronic nonbacterial osteomyelitis is an autoimmune disorder that causes bone inflammation. What causes the condition is unknown, as no bacteria or infection are present when inflammation occurs.
Juvenile idiopathic arthritis is a chronic disease with no known cause. There are different forms of the condition, which can affect one or more joints at a time and may also affect the skin and eyes.
Systemic lupus erythematosus is a rare, chronic autoimmune condition that can affect different parts of the body, such as the kidneys, skin, joints and blood.
Juvenile dermatomyositis is an autoimmune condition most often diagnosed in children between the ages of 4 and 10. The disease leads to inflammation in tiny blood vessels in the muscles (myositis) and skin (dermatitis).
Overlap syndrome refers to patients diagnosed with an autoimmune rheumatic disease that cannot easily be identified as a known condition — such as lupus or juvenile arthritis — because symptoms and signs or more than one condition are present.
Vasculitis is the inflammation of blood vessels, causing poor blood flow to tissues (lungs, kidneys, skin) in the body. There are many forms of this rare condition, which vary widely in symptoms.
Systemic autoinflammatory diseases are a new category of rheumatic and inflammatory conditions that differ from lupus and juvenile arthritis. SAIDs are inherited genetic conditions often involving fever syndromes.
Periodic Fever Syndrome refers to a group of autoimmune inflammatory conditions with similar symptoms. The main sign is a recurrent fever when there is no infection.
The expert rheumatology doctors, nurses and physical therapists at Arkansas Children’s are highly trained to treat a wide range of pediatric arthritis and rheumatic conditions. Our team provides your child with the most advanced treatment and is here to answer your questions.
Rheumatology
Little Rock, Springdale
Rheumatology
Little Rock, Springdale
Rheumatology
Little Rock, Springdale
Otolaryngology (Ear, Nose, Throat)
Little Rock, Springdale
Rheumatology
Little Rock, Springdale
An Arkansas Children's Podcast is about the people, places, and programs of Arkansas Children's. Podcasts are available monthly on Apple Podcasts and Google Podcasts.
Our team provides the most advanced care and many of our doctors, nurses and staff are actively involved in research to improve care outcomes and find new treatments for these often difficult-to-manage conditions.
Possible treatments include:
These research studies were started by faculty members and doctors at Arkansas Children’s.
Our chaplains are on staff to assist all patients and families from any faith background with religious and spiritual needs.
Child Life reduces stress and promotes positive coping using developmentally appropriate preparation, education, and play at Arkansas Children's.
Arkansas Children's offers on-site dining, shuttle services, and gift shops, as well as discounted hotels and rv parks nearby.
Use these resources to learn more about pediatric arthritis and other rheumatic diseases.
Information and videos for patients and caregivers pertaining to rheumatic conditions.
Worldwide group providing condition-specific information and resources for a variety of rheumatic illnesses.
Organization dedicated to providing information and support to families living with juvenile arthritis.
Our app is designed to be your "go-to" for managing your child's health day or night.
Arkansas Children's has an online bill pay system to pay your bill for visits and admissions.
Manage your child's medical information and connect with your Arkansas Children's medical team anytime online!
Log in to MyChartArkansas Children's offers translation assistance to the hearing impaired as well as non-English speaking patients and families.
Access the information and tools you need to stay connected with Arkansas Children's quickly.