Measles in Arkansas: What You Need to Know Click here for more information >
Measles in Arkansas: What You Need to Know Click here for more information >

Ranked nationally in pediatric care.
Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2024-2025.

It's easier than ever to sign up for MyChart.
Sign up online to quickly and easily manage your child's medical information and connect with us whenever you need.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

When it comes to your child, every emergency is a big deal.
Our ERs are staffed 24/7 with doctors, nurses and staff who know kids best – all trained to deliver right-sized care for your child in a safe environment.

Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2024-2025.

Looking for resources for your family?
Find health tips, patient stories, and news you can use to champion children.

Support from the comfort of your home.
Our flu resources and education information help parents and families provide effective care at home.

Children are at the center of everything we do.
We are dedicated to caring for children, allowing us to uniquely shape the landscape of pediatric care in Arkansas.
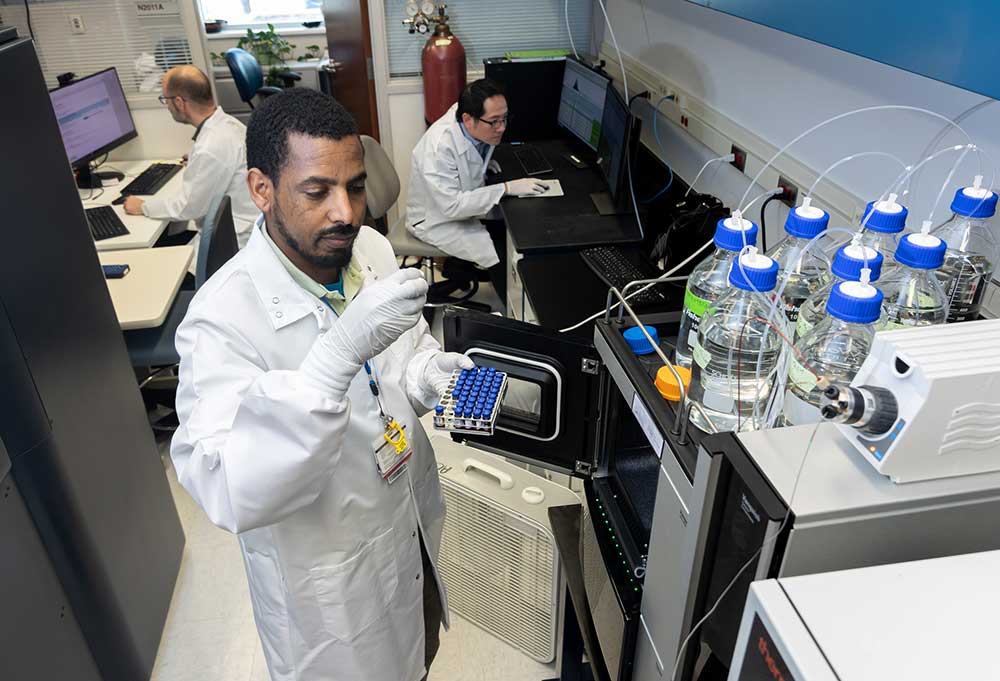
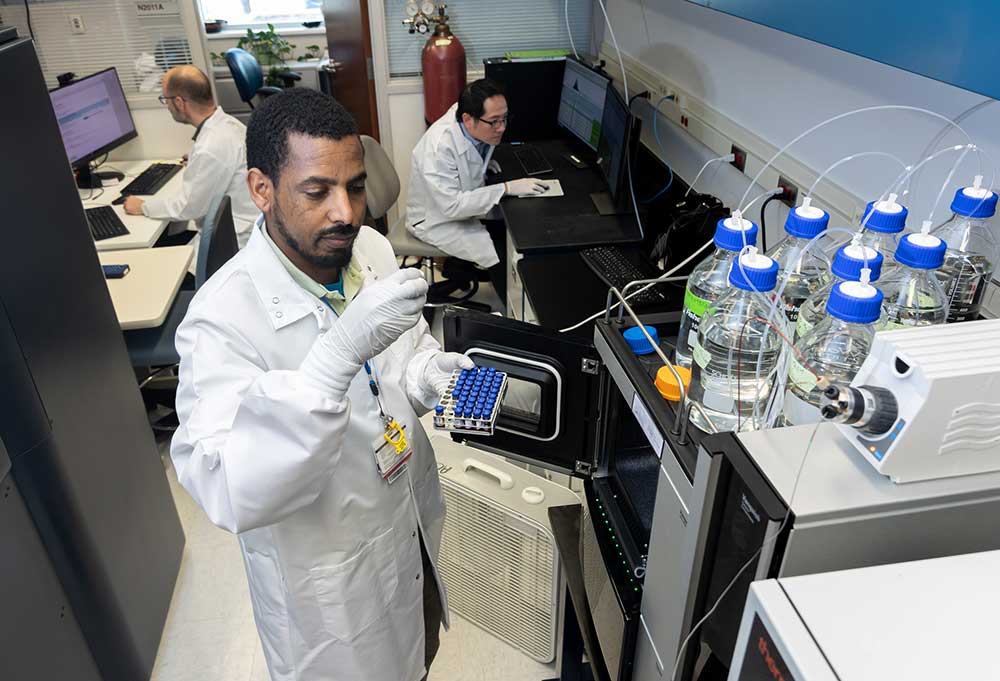
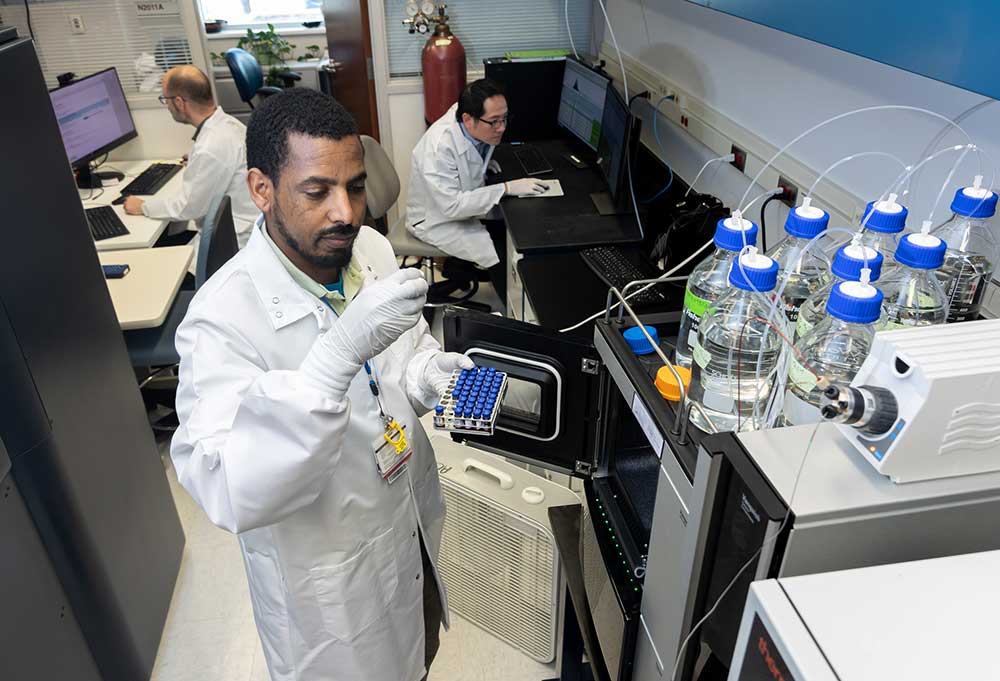
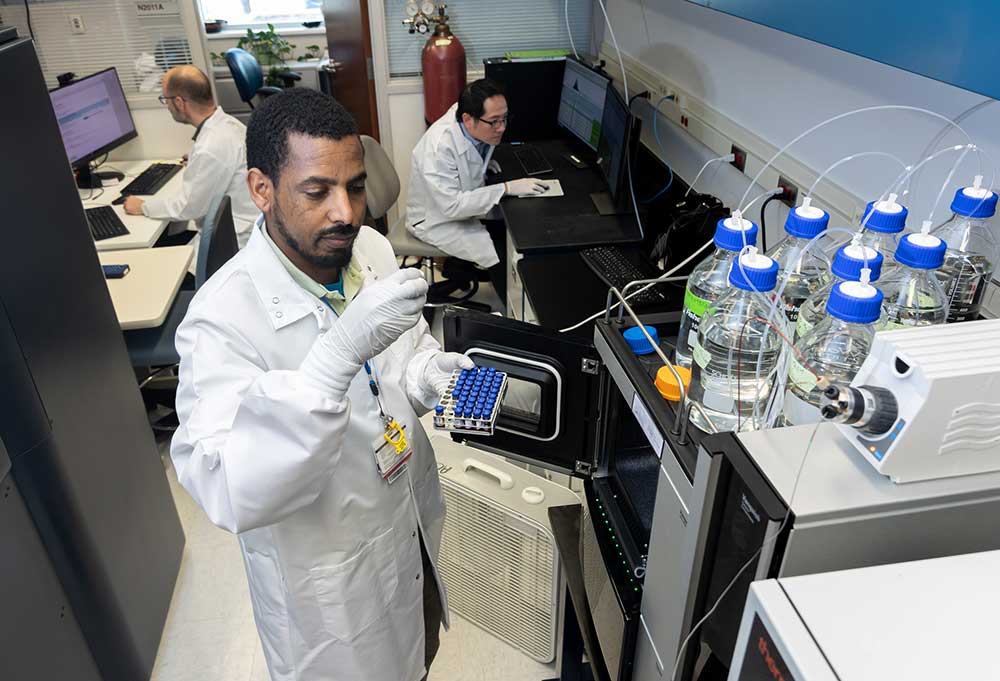
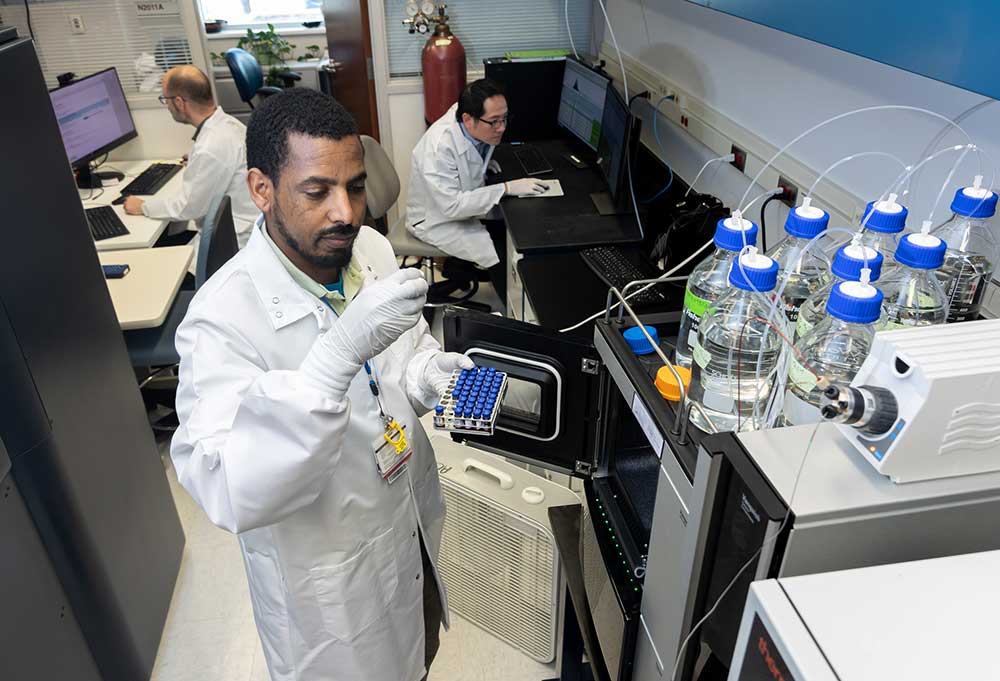
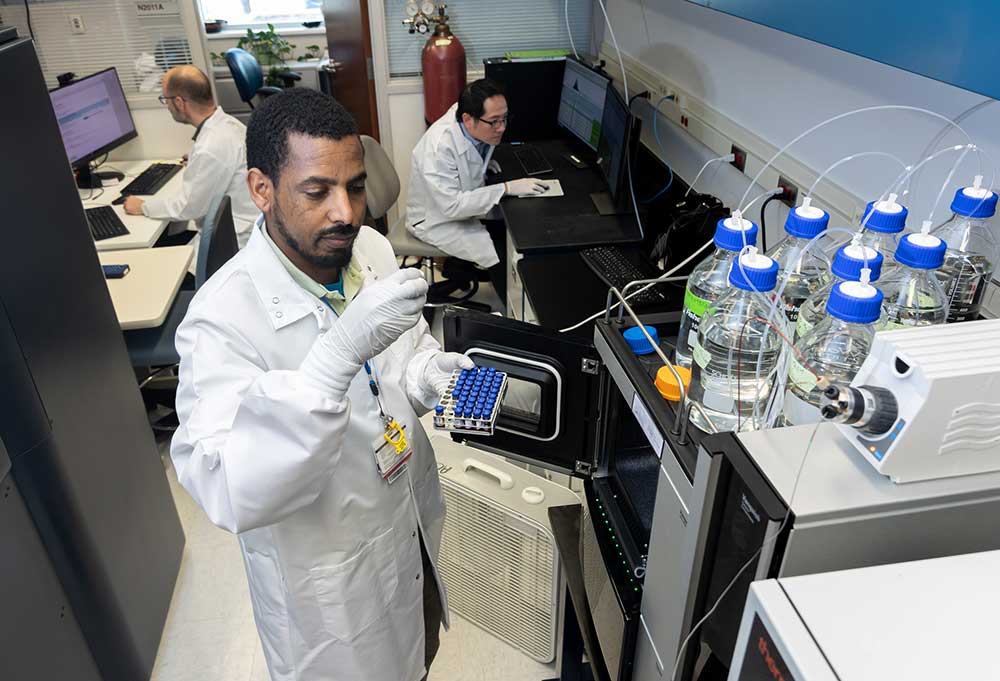
Transforming discovery to care.
Our researchers are driven by their limitless curiosity to discover new and better ways to make these children better today and healthier tomorrow.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

Then we're looking for you! Work at a place where you can change lives...including your own.

When you give to Arkansas Children's, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond

Become a volunteer at Arkansas Children's.
The gift of time is one of the most precious gifts you can give. You can make a difference in the life of a sick child.

Join our Grassroots Organization
Support and participate in this advocacy effort on behalf of Arkansas’ youth and our organization.
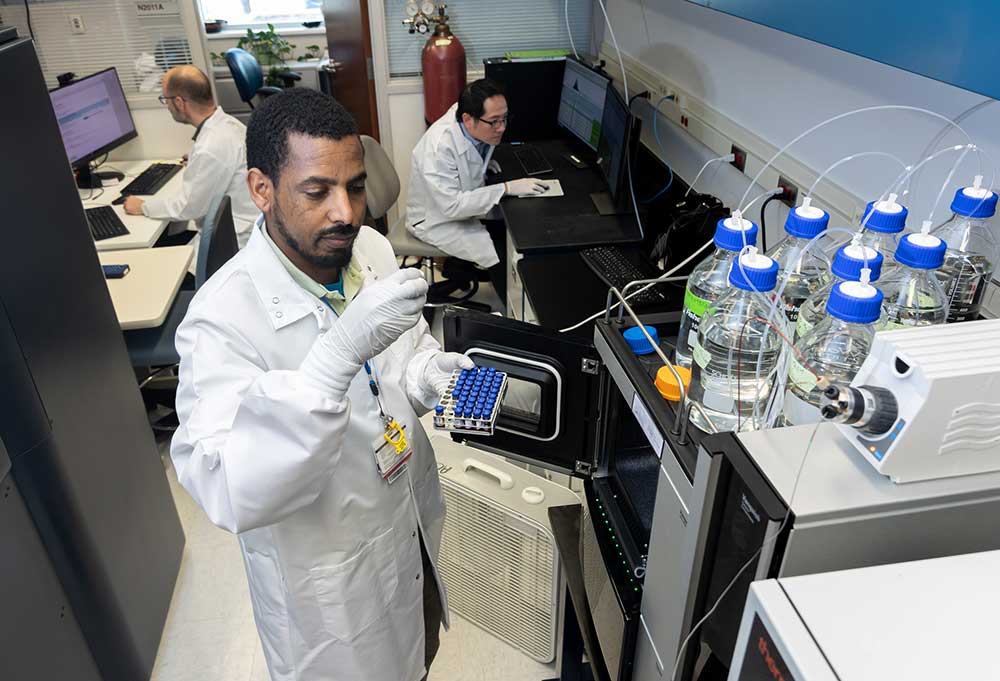
Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.
Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.
Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.
Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.
Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.
Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

When you give to Arkansas Children’s, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond.

Your volunteer efforts are very important to Arkansas Children's. Consider additional ways to help our patients and families.

Join one of our volunteer groups.
There are many ways to get involved to champion children statewide.

Make a positive impact on children through philanthropy.
The generosity of our supporters allows Arkansas Children's to deliver on our promise of making children better today and a healthier tomorrow.

Read and watch heart-warming, inspirational stories from the patients of Arkansas Children’s.
Hello.
Arkansas Children's Hospital
General Information 501-364-1100
Arkansas Children's Northwest
General Information 479-725-6800

Our specialists provide pediatric care across the state and region to make children better today and healthier tomorrow.
Request Appointment
Arkansas Children’s Hospital has again received the highest international recognition for excellence in nursing, achieving redesignation as a Magnet® hospital on Wednesday.
Just 8 percent of U.S. health care organizations earn Magnet® designation, widely considered the highest international credential for professional nursing practice and signifying excellence in clinical care.
Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2024-2025.

Cappy and Charlie Whiteside have generously donated $1 million toward Arkansas Children’s Hospital’s historic expansion.
Robin and Gary George and family have generously donated $1 million toward Arkansas Children’s Hospital’s historic expansion project.
Arkansas Children’s Northwest (ACNW) has appointed healthcare leader and endocrinologist Ryan McDonough, D.O., FAAP, as its new chief medical officer.
A phase I open-label trial to assess the tolerability and safety of an up-dosing regimen with a once-daily peanut SLIT-tablet in adults, adolescents, and children with peanut allergy.
This study is looking at risk factors for food allergies and eczema in young children.
Learn more about the HBCD Study, sponsored by the National Institutes of Health, the largest long-term study of early brain and child development in the United States.
Read about Dr. Adrienne Koder, an accomplished skier and a pediatric orthopedic surgeon, operating room medical director and secretary of staff at Arkansas Children's Northwest in Springdale.
Arkansas Children’s Neurogastroenterology and Motility Program focuses on diagnosing and treating chronic GI issues in children. Our team understands the challenges of gut-brain interaction disorders, offers innovative diagnostic methods and provides a multidisciplinary approach to management.
Learn more about the challenges and highlights of pediatric health care photography with this glimpse into a day in the life of Arkansas Children’s photographer John David Pittman.
We know that healthcare can be complicated, so we make it as easy as possible to access primary and specialty care.